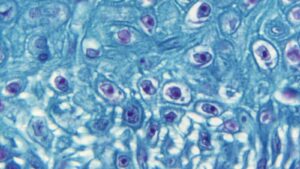
As soon as the world hoped to say goodbye to COVID-19, some Monkeypox-infected infections appear to be spreading around the world. About 100 Monkeypox cases have been identified in more than 12 countries. Monkeypox is a zoonotic description that spreads from animals to humans. It is caused by the Orthopox virus which is very similar to smallpox but is usually softer. This spread mainly through skin-to-skin contact but researchers are also looking for alternative means of transmission, given the sudden increase in cases across Europe and other countries.
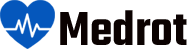
The incubation period is longer compared to smallpox from 5 to 21 days. It starts with fever, chills, headache, chills, muscle aches, and loss of appetite and within 5 days scratches and sores appear. The rashes first appeared on the face and later spread throughout the body.

Symptoms of monkey Vs and symptoms of smallpox
The symptoms of monkeypox are very similar to the symptoms of chickenpox, making it difficult to distinguish between them. The monkey’s bubble is usually larger than smallpox. The sores last from one week to 3 weeks, usually allowing them to separate until the last skin lesions have dried, fallen, and healed. People with Smallpox often develop swollen lymph glands in the neck and are prone to touch / testing. It is mainly a chronic disease that lasts anywhere between 1 to 3 weeks. It is considered an average risk to public health with an average mortality rate of between 1 and 10 percent. It can be controlled by separation, proper skin care, and antimicrobials.
Monkeypox can be passed from person to person, but it is rare. When a person comes in contact with the virus particles from another person, this is known as human-to-human transmission (transmission). The virus can be spread by airborne droplets when an infected person coughs or sneezes. Although you need to come face to face with it for a long time, you can breathe these tiny drops from another person (breath drops) or apply them to your eyes or nose. You can get it by touching the wounds of an infected person.

Should we get a smallpox vaccine?
A smallpox vaccine can be given to people who have been exposed to suspected or confirmed cases at the Monkeypox clinic. In India there are currently no confirmed cases of Monkeypox, with the Government of India issuing guidelines to address this, samples of suspects from all over the country are still being prepared at the National Infectious Diseases Center. In the current situation, there is no need to alarm or collect antivirals. Vaccines on demand are not given indiscriminately and infants are prescribed for those exposed to suspicious or confirmed Monkeypox conditions. Properly covered, it will withstand a great deal of adverse conditions.
ACAM200 and JYNNEOSTM (also known as Imvamune or Imvanex) are two licensed drugs currently in the United States to prevent smallpox.
Pre-exposure prophylaxis to prevent monkeys
The Immunization Advisory Committee (ACIP) recommends that people whose activities may expose them to orthopoxviruses, such as monopolypox, be vaccinated with ACAM2000 or JYNNEOS to protect them if they are exposed to orthopoxvirus. This is known as pre-exposure prophylaxis (PrEP). People who should receive PrEP include:
Clinical laboratory staff conducting tests to detect orthopoxviruses, including those using polymerase chain reaction (PCR) tests to detect orthopoxviruses, including the Monkeypox virus.
Research laboratory staff directly dealing with cultures or animals contaminated with or infected with orthopoxviruses that infect humans, including the Monkeypox virus, the Vaccinia virus that is reproducible, or recurrent Vaccinia viruses are found in a variety of Vaccinia viruses that are reproducible.
Certain members of the health care and community health team have been appointed by the public health authorities for immunization purposes.
People who can get PrEP if they want to get it include health workers who give ACAM2000 or who expect to care for more patients with pox.

At this time, many doctors in the United States and laboratory staff who did not perform an orthopoxvirus generic test to diagnose orthopox viruses, including monotheypox, were advised to receive orthopoxvirus PrEP. Laboratory experts should consult with biosafety officials and laboratory authorities to determine the risks and safety measures, depending on the type of work they are doing. Whether they receive PrEP, physicians and laboratories should use recommended methods of infection control; these are important in preventing any infection.
ACAM2000 is used as a preparation for live Vaccinia virus that is vaccinated against the skin by scratching the skin. Following a successful vaccination, the wound will grow in place of the vaccine (i.e., “take”). The virus that grows in the area of this injection can spread to other parts of the body or to other people. People receiving the ACAM2000 vaccine should take steps to prevent the spread of the vaccine and be considered vaccinated within 28 days.
JYNNEOSTM is administered as a non-repetitive living virus. Inject as two subcutaneous injections four weeks apart. There is no apparent “taking” and as a result, there is no risk of transmission to other parts of the body or to other people. People receiving JYNNEOSTM are not considered vaccinated for up to 2 weeks after receiving the second dose of the vaccine.
The CDC, in conjunction with the Immunization Advisory Committee (ACIP), provides recommendations on who should receive smallpox vaccination in a non-emergency environment. At this time, vaccination with ACAM2000 is recommended in laboratories that work with specific orthopoxviruses and antibodies. On November 3, 2021, ACIP voted to recommend JYNNEOS pre-exposure prophylaxis as an alternative to ACAM2000 for certain individuals at risk of exposure to orthopoxviruses.
Application of the Policy
Because the monopoly virus is closely related to the virus that causes smallpox, smallpox vaccine can protect humans from being infected with monkeys. Previous data from Africa suggests that the smallpox vaccine is at least 85% effective in preventing monkeys. The efficacy of JYNNEOSTM versus monypoxy was concluded in clinical studies regarding JYNNEOS immunogenicity and efficacy data from animal studies.
Smallpox vaccines and monkeypox vaccines are effective in protecting people from pox if given before exposure to monkeypox. Experts also believe that vaccination after exposure to monopolypox may help prevent the disease or make it worse.
Getting Vaccinated After Exposure to Monkeypox Virus

The sooner the target person gets the goal, the better.
The CDC recommends that vaccination be given within 4 days from the date of exposure to prevent the onset of the disease. If given within 4-14 days after exposure, vaccination may reduce the symptoms, but it may not prevent the disease.
The doctor demonstrates the use of a double needle during the 2002 Smallpox Vaccine Workshop.
Smallpox vaccines and monkeypox vaccines are effective in protecting people from pox if given before exposure to monkeypox. Experts also believe that vaccination after exposure to monopolypox may help prevent the disease or make it worse.
Recovery After Exposure
People who have been exposed to the monopoly virus and who have not been vaccinated for the past 3 years should consider vaccination.
The sooner a person gets a vaccine, the better it will be for protecting the moxox virus.
Risks of Immunization against Monkeypox Disease
For most people who are exposed to monsters, the risk of mummypox disease is greater than the risk of smallpox or monkey vaccine.
Monkey is a dangerous disease. It causes fever, headache, muscle aches, back pain, swollen lymph nodes, general feeling of discomfort, fatigue and severe rashes. A study of monkeypox in Central Africa — where people live in isolation and poor health care — has shown that the disease has killed at least 11% of the population.
In contrast, most people who receive a vaccine for smallpox or monkey have only a mild reaction, such as a slight fever, fatigue, swollen glands, redness and itching in the area where the vaccine is given. However, these vaccines have serious risks, too.