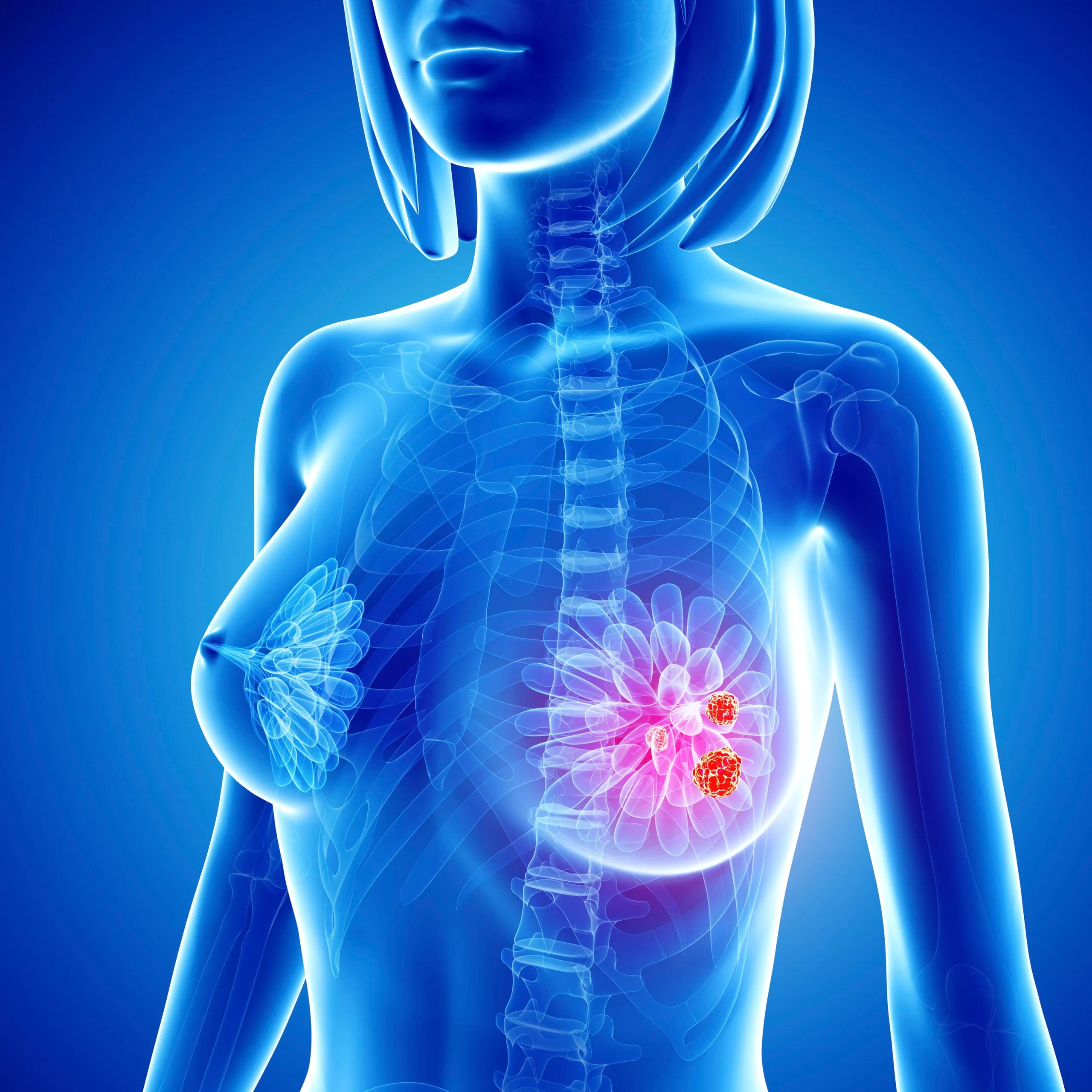
Cancer occurs when mutations are called genetic mutations that control cell growth. Modification allows cells to differentiate and replicate in an uncontrolled manner.
Breast cancer is a cancer of the breast cells. Usually, the cancer develops in the lobules or in the fallopian tubes.
Lobles are glands that produce milk, and the ducts are the way milk is released from the nipple. Cancer can also occur in fatty tissue or fibrous connective tissue inside your breast.
Uncontrolled cancer cells often invade other healthy breast tissue and can travel to the lymph nodes under the arms. Lymph nodes are a key mechanism that helps cancer cells move to other parts of the body.
Signs and symptoms of breast cancer
In its early stages, breast cancer may not cause any symptoms. In most cases, the tumor may be too small to be felt, but abnormalities may still be seen in the mammogram.
If the tumor is not felt, the first sign is usually a new lump in the breast that was not there before. However, not all lumps are cancerous.
Each type of breast cancer can cause a variety of symptoms. Many of these symptoms are similar, but some may be different. The most common symptoms of breast cancer include:
A lump of breast or thickening of tissue that feels different from the surrounding and newly formed tissue
Breast pain Red skin, with pores on the rest of your breast
Swelling throughout or part of your breast
Nipple discharge without breast milk
Bleeding from your nipple
Peeling, stretching, or peeling of the skin on your nipple or breast
A sudden, unexplained change in the shape or size of your breast
distorted nipple
Changes in the appearance of the skin on your breasts
lump or swelling under your arm
If you have any of these symptoms, it does not mean that you have breast cancer. For example, pain in your chest or breast can be caused by a benign cyst.
However, if you find a lump in your breast or other symptoms, you should see your doctor for a checkup.
Types of breast cancer
There are several types of breast cancer, and they are divided into two main categories: “invasive” and “noninvasive,” or in situ.
Although invasive cancers have spread from the mammary glands or glands to other parts of the breast, rare cancers do not spread from the original tissue.
These two categories are used to describe the most common types of breast cancer, including:
Ductal carcinoma in situ. Ductal carcinoma in situ (DCIS) is a rare condition. With DCIS, the cancer cells are trapped in the bones in your breast and did not invade the surrounding breast tissue.
Lobular carcinoma in situ. Lobular carcinoma in situ (LCIS) is a cancer that grows in the mammary glands of your breast. Like DCIS, cancer cells did not invade surrounding tissues.
Invasive ductal carcinoma. Invasive ductal carcinoma (IDC) is the most common type of breast cancer. This type of breast cancer starts in the lining of your breast milk and attacks the tissues around the breast. Once breast cancer has spread to the tissue outside your milk ducts, it can begin to spread to other organs near the tissues.
Infectious lobular carcinoma. Inflammatory lobular carcinoma (ILC) begins to grow in the lobes of your breast and attacks nearby tissues.
Other, more common types of breast cancer include:
Paget’s nipple infection. This type of breast cancer starts in the arteries of the nipple, but as it grows, it begins to affect the skin and nipple aola.
Phyllodes tumor. This rare form of breast cancer develops in the breast tissue. Most of these plants are harmless, but some have cancer.
Angiosarcoma. This is a cancer that grows in the blood vessels or lymph nodes in the breast.
The type of cancer you have determines your treatment options, as well as your long-term outcome.
Doctors know that breast cancer occurs when some of the breast cells begin to grow abnormally. These cells divide more quickly than healthy cells and continue to accumulate, forming a lump or mass. Cells may spread metastasize from your breast to your lymph nodes or to other parts of your body.
Causes
Breast cancer usually begins with cells in the milk ducts (invasive ductal carcinoma). Breast cancer can also be started in an invasive lobe or invasive lobby carcinoma or in other cells or tissues within the breast.
Researchers have identified hormones, lifestyle, and environmental factors that may increase your risk of breast cancer. But it is not clear why some harmless people get cancer, but some vulnerable people have never had it. Breast cancer is more likely to be caused by complex genetic factors.
Doctors estimate that about 5 to 10 percent of breast cancers are related to genetic mutations in previous generations.
Inherited Breast Cancer
A number of modified genes that can increase the risk of breast cancer have been identified. The best known are breast cancer gene 1 (BRCA1) and breast cancer gene 2 (BRCA2), both of which increase the risk of both breast and cervical cancer.
If you have a strong family history of breast cancer or other cancers, your doctor may recommend a blood test to help identify certain mutations in BRCA or other genes passed on to your family.
Consider asking your doctor to refer you to a genetic counselor, who can review your family health history. The genetic counselor can also discuss the benefits, risks and limitations of genetic testing to help you make informed decisions.
The risk factor for breast cancer is anything that makes you more likely to get breast cancer. But having one or more risk factors for breast cancer does not mean that you will have breast cancer. Most women who get breast cancer have no known risk factors other than being women.
Factors associated with an increased risk of breast cancer include
- Being a woman- Women are more likely to get breast cancer than men.
- Growth of years-Your chances of getting breast cancer increase as you get older.
- Personal history of breast conditions-If you have had a breast biopsy that has detected lobular carcinoma in situ (LCIS) or atypical hyperplasia of the breast, you have an increased risk of breast cancer.
- Personal history of breast cancer-If you have had breast cancer in one breast, you have an increased risk of developing breast cancer.
- Family history of breast cancer- If your mother, sister or daughter is diagnosed with breast cancer, especially as a young child, the risk of developing breast cancer increases. However, most people who are diagnosed with breast cancer do not have a family history of the disease.
- Genetics that increase the risk of cancer-Genetic modifications that increase the risk of breast cancer can be passed from parents to children. The most well-known genetic mutations are called BRCA1 and BRCA2. These genes can significantly increase the risk of breast cancer and other cancers, but they do not prevent cancer.
- Radiation exposure-If you have received radiation therapy for your chest as a child or a young adult, your chances of getting breast cancer increase.
- Obesity-Obesity increases the risk of breast cancer.
- Starting your period at a young age- Starting your period before 12 years increases the risk of breast cancer.
- The onset of menopause in adulthood.-If you start menstruating when you are older, you are more likely to get breast cancer.
- Having your first child when you grow up-Women who give birth to their first child after 30 years may have an increased risk of breast cancer.
- She has never been pregnant-Women who have never been pregnant are at a higher risk of developing breast cancer than women who have had one or more pregnancies.
- Postmenopausal hormone treatment-Women who use hormone therapy that includes estrogen and progesterone to treat the signs and symptoms of menopause have an increased risk of breast cancer. The risk of developing breast cancer decreases when women stop taking these drugs.
- Drinking alcohol-Drinking alcohol increases the risk of breast cancer.
Making changes in your daily life may help reduce the risk of breast cancer. Try to :-
Ask your doctor about breast cancer screening. Talk to your doctor when to start breast cancer screening and testing, such as clinical breast screening and mammograms.
- Talk to your doctor about the benefits and risks of testing. Together, you can decide which breast cancer screening strategies are best for you.
- Get acquainted with your breasts by examining your breasts for breast awareness-Women may choose to get acquainted with their breasts by checking their breasts from time to time for self-examination. If there are any new changes, lumps or other unusual symptoms in your breasts, talk to your doctor right away.
- Breast awareness can not prevent breast cancer, but it may help you to better understand the common changes your breasts are experiencing and to recognize any unusual signs and symptoms.
- Drink alcohol in moderation-Limit the amount of alcohol you drink to no more than one drink per day, if you choose to drink.
- Exercise several days a week-Schedule at least 30 minutes of physical activity on most days of the week. If you have been unemployed recently, ask your doctor if it is okay and start small.
- Reduce postmenopausal hormone treatment-Combined hormone therapy may increase the risk of breast cancer. Talk to your doctor about the benefits and risks of hormone replacement therapy.
- Some women experience disturbing signs and symptoms during menopause and, for these women, an increased risk of breast cancer may be justified in reducing the signs and symptoms of menopause.
- To reduce the risk of breast cancer, use a very low dose of hormone therapy in a very short time.
- Maintain a healthy weight. If your weight is healthy, work to maintain that weight. If you need to lose weight, ask your doctor about healthy strategies to achieve this. Reduce the amount of calories you eat each day and gradually increase the amount of exercise.
- Choose healthy foods. Women who eat a Mediterranean diet mixed with extra-virgin olive oil and mixed nuts may have a lower risk of breast cancer. The Mediterranean diet focuses on plant-based foods, such as fruits and vegetables, whole grains, cereals, and nuts. People who follow the Mediterranean diet prefer healthy fats, such as olive oil, over butter and fish instead of red meat.
Reducing the high risk of breast cancer in women
- If your doctor examines your family history and determines if you have any other factors, such as breast cancer, which may increase your risk of breast cancer, you may want to discuss options for reducing your risk, such as:
- Estrogen-blocking drugs, such as selective estrogen receptor modulators and aromatic inhibitors, reduce the risk of breast cancer in women at high risk of the disease.
- These drugs carry the risk of side effects, so doctors keep these drugs in women who are at a higher risk of breast cancer. Discuss the pros and cons with your doctor.
- Preventive surgery. Women who are at a higher risk of developing breast cancer may choose to have their breasts removed by surgery (prophylactic mastectomy). They may also choose the removal of their healthy eggs (prophylactic oophorectomy) to reduce your risk of both breast cancer and cervical cancer.
Burning breast cancer
Inflammatory breast cancer (IBC) is a rare but aggressive form of breast cancer. IBC only makes between 1 and 5 percent Reliable Source for all breast cancer cases.
In this case, the cells block the lymph nodes near the breast, so the lymph vessels in the breast are unable to excrete properly. Instead of creating a tumor, IBC causes your breast to swell, look red, and feel very warm. A breast cancer may look hollow and thick, like an orange peel.
IBC can be very aggressive and can develop rapidly. For this reason, it is important to call your doctor immediately if you notice any symptoms.
Find out more about IBC and the symptoms it can cause.
Metastatic breast cancer
Metastatic breast cancer is another name for stage 4 breast cancer. Prostate cancer is spread from your breast to other parts of your body, such as your bones, lungs, or liver.
This is an advanced stage of breast cancer. Your oncologist (cancer doctor) will develop a treatment plan to stop the growth and spread of the tumor.
Learn about the treatment options for metastatic cancer, as well as the factors that affect your vision.
Triple-negative breast cancer
Triple-negative breast cancer is another rare form of the disease, affecting only 10 to 15 percent of the Reliable Source of Breast Cancer, according to the American Cancer Society (ACS).
To diagnose triple-negative breast cancer, the tumor must have the following three characteristics:
- It has no estrogen receptors. These are receptors on cells that bind, or attach to, the hormone estrogen. When a tumor contains estrogen receptors, estrogen can stimulate cancer to grow.
- It does not have progesterone receptors. These cellular receptors bind to the hormone progesterone. If the tumor contains progesterone receptors, progesterone can stimulate cancer to grow.
- It has no extra HER2 protein in its surface. HER2 is a protein that stimulates the growth of breast cancer.
- When a tumor meets these three mechanisms, it is called triple breast cancer. This type of breast cancer usually grows and spreads faster than other types of breast cancer.
Triple-negative breast cancer is difficult to treat because hormone cancer treatment does not work.
Learn about the treatment and survival rates of triple breast cancer.
Stages of breast cancer
Breast cancer can be divided into stages according to the size of the tumor and the extent of its spread.
Major cancers and / or invasions of nearby tissues or advanced organs are less common and / or still in breast cancer. To cause breast cancer, doctors need to know :-
If the cancer is invading or non-invasive
How big is the tumor
Whether lymph nodes are involved
If the cancer has spread to nearby tissue or organs
Breast cancer has 5 main stages: stages 0 to 5.
Category 0 breast cancer
Stage 0 is DCIS. Cancer cells in DCIS remain trapped in the mammary glands and do not spread to nearby tissues.
Stage 1 of breast cancer
Stage 1A: The main tumor is 2 cm (cm) wide or less, and the lymph nodes are unaffected.
Stage 1B: The cancer is found in nearby lymph nodes, and there may be no tumor in the breast, or a tumor smaller than 2 cm.
Stage 2 breast cancer
Stage 2A: The tumor is smaller than 2 cm and has spread to nearby nearby lymph nodes 1–3, or is between 2 and 5 cm and has never spread to any lymph nodes.
Stage 2B: The tumor is between 2 and 5 cm and has spread to 1–3 axillary lymph nodes (armpits), or larger than 5 cm and has never spread to any lymph nodes.
Stage 3 of breast cancer
Section 3A:
The cancer has spread to 4-9 axillary lymph nodes or enlarged internal lymph nodes, and the main tumor can be of any size.
The abscesses are larger than 5 cm, and the cancer has spread to 1-3 axillary lymph nodes and any nodes of the breast.
Stage 3B: The tumor has penetrated the chest wall or skin and may not have infected up to nine lymph nodes.
Stage 3C: Cancer is found in 10 or more lymph nodes, lymph nodes near the collarbone, or internal mammary nodes.
Stage 4 breast cancer
Stage 4 of breast cancer can be tumors of any size, and its cancer cells are spread to nearby and distant lymph nodes and organs.
Checking with your doctor will determine the stage of your breast cancer, which will affect your treatment.
Male breast cancer
Although they usually have a smaller one, men have breast tissue like women. Men can get breast cancer too, but it is very rare.
According to ACS Trusted Source, breast cancer is 100 times more common in white men than in white women. It is 70 times more common in black men than in black women.
That being said, breast cancer in men is dangerous as it is found in women with breast cancer. It also has the same symptoms.
Learn more about breast cancer in men and the symptoms you should look for.
Breast cancer survival rate
Breast cancer cell survival rates vary greatly based on many factors.
The two most important factors are the type of cancer you have and the stage of the cancer when you get the diagnosis. Other factors that may be involved include your age, gender, and race.
Research Trusted Source shows that the death rate for non-whites with breast cancer is higher than for whites. One reason for this may be the disparity in health care.
The good news is that breast cancer survival rates are improving.
According to ACS Trusted Source, in 1975, the five-year survival rate for breast cancer in women was 75.2%. But of the women diagnosed between 2008 and 2014, it was 90.6 percent.
The five-year survival rate of breast cancer varies depending on the stage of diagnosis, ranging from 99 percent of local, first-stage cancer to 27 percent of metastatic cancers.
Find out more about survival statistics and the factors that affect them.
Breast cancer diagnosis
To determine if your symptoms are caused by breast cancer or a benign breast cancer, your doctor will perform a more complete physical examination than a breast examination. They may also request one or more diagnostic tests to understand what is causing your symptoms.
Tests that can help detect breast cancer include:-
Mammogram– The most common way to see under your chest is an image test called a mammogram. Many women in their 40s and older receive an annual mammograms to test for breast cancer. If your doctor suspects that you have a tumor or a suspicious area, he or she will also request a mammogram. If an abnormal area appears in your mammogram, your doctor may request further tests.
Ultrasound-Breast ultrasound uses sound waves to create a tissue image at the depth of your breast. An ultrasound can help your doctor distinguish between a solid mass, such as a tumor, and a benign cyst.
Your doctor may also recommend tests such as an MRI or breast biopsy.
Learn about other tests that can be used to detect breast cancer.
If you do not yet have a primary care physician, you can check with your local doctor with the Healthline FindCare tool.
Breast biopsy
If your doctor suspects breast cancer, he or she may order both a mammogram and an ultrasound. If both tests do not tell your doctor that you have cancer, your doctor may have a breast biopsy.
During this test, your doctor will remove a tissue sample from the suspicious area for testing.
There are several types of breast biopsy. For one of these tests, your doctor uses a needle to take a tissue sample. Some, they cut your chest and take out a sample.
Your doctor will send a tissue sample to the laboratory. If the sample is found to be cancer-free, the lab can test it again to tell your doctor what type of cancer you have.
Learn more about breast biopsy, how to prepare one, and what to expect.
Treatment of breast cancer
The stage of your breast cancer, how far you have advanced (if you have had it), and how advanced the tumor is all play a part in deciding what kind of treatment you need.
First, your doctor will determine your cancer size, stage, and distance (how likely it is to grow and spread). Then you can discuss your treatment options.
Surgery is the most common treatment for breast cancer. Many people have alternative therapies, such as chemotherapy, targeted therapy, radiation therapy, or hormone replacement therapy.
Surgery
Several types of surgery can be used to remove breast cancer, including:-
- Lumpectomy-This process removes the tumor and other surrounding tissues, leaving the entire breast intact.
- Mastectomy-In this procedure, the surgeon removes the entire breast. In a double mastectomy, both breasts are removed.
- Sentinel node biopsy-This surgery removes several lymph nodes that receive fluid from the plant. These lymph nodes will be tested. If they do not have cancer, you may not need further surgery to remove most of the lymph nodes.
- Axillary lymph node dissection– If the lymph nodes are removed during a sentinel node biopsy containing cancer cells, your doctor may remove the extra lymph nodes.
- Contralateral prophylactic mastectomy-Although breast cancer may be present in only one breast, some people prefer to have a contralateral prophylactic mastectomy. This surgery removes your healthy breast to reduce the risk of developing breast cancer again.
Radiation therapy
In radiation therapy, high-dose radiation is used to identify and kill cancer cells. Many radiotherapy treatments use external beam radiation. This method uses a large machine outside the body.
Advances in cancer treatment have enabled doctors to diagnose cancer internally. This type of radiation therapy is called brachytherapy.
To perform brachytherapy, surgeons place radiation pellets, or pellets, inside the body near the plant surface. The seeds remain there for a short time and work to destroy cancer cells.
Chemotherapy
Chemotherapy is a drug that is used to destroy cancer cells. Some people may be treated with chemotherapy on their own, but this type of treatment is often used in conjunction with other therapies, especially surgery.
In some cases, doctors prefer to give their patients chemotherapy before surgery. The hope is that treatment will reduce the tumor, then surgery will not be necessary to attack.
Chemotherapy has many unwanted side effects, so talk to your doctor about your concerns before starting treatment.
Hormone therapy
If your breast cancer is sensitive to hormones, your doctor may prescribe hormone replacement therapy. Estrogen and progesterone, two female hormones, can stimulate the growth of breast cancer cells.
Hormone therapy works by blocking your body’s production of these hormones or by blocking hormone receptors in cancer cells. This action can help slow down and possibly stop the growth of your cancer.
Medications
Certain therapies are designed to target specific abnormalities or mutations in cancer cells.
For example, Herceptin (trastuzumab) can inhibit your body’s production of the HER2 protein. HER2 helps breast cancer cells grow, so taking medication to reduce the production of this protein can help slow cancer growth.
Your doctor will tell you more about any specific treatment he or she recommends.
Lifestyle factors can affect your risk of breast cancer
For example, overweight women are at greater risk of developing breast cancer. Maintaining a healthy diet and exercising as often as possible can help you lose weight and reduce your risk.
Alcohol abuse also increases your risk. This could be drinking more than two drinks a day or indulging in alcohol.
However, a report that analyzes worldwide has shown that even one drink a day increases the risk of breast cancer. If you drink alcohol, talk to your doctor about the amount they recommend.
Breast cancer screening
Regular mammograms may not prevent breast cancer, but they may help to reduce the risk of developing undiagnosed cancers.
The American College of Physicians (ACP) offers the following general recommendations for women at risk for moderate breast cancer:
Women 40 to 49: It is not recommended to do an annual mammogram, but women should discuss their preferences with their doctors.
Women 50 to 74 years: It is recommended to have a mammogram every year.
Women 75 years and older: Mammograms are no longer recommended.
ACP also recommends anti-mammograms for women living 10 years or less.
These are just guidelines.
Recommendations from ACS vary. According to ACS, women should have the option to get an annual test at the age of 40, start an annual exam at the age of 45, and move on to a two-year test at the age of 55.
The specific recommendations for mammograms are different for each woman, so talk to your doctor to see if you should get a normal mammogram.
This is all about breast cancer.
